In Ontario, every patient who cannot make decisions for themselves has a Substitute Decision Maker (SDM). The ICU team legally can share information with the SDM or Power of Attorney (POA) only and the role of SDM or POA is to make decisions if the patient is incapable. In this way, we ensure that the patient’s privacy is protected. We trust that SDM/POA decides how they will share information about their loved one with the rest of the family. If there are multiple SDMs, we ask them to decide who will be the contact person, so the continuity of information is maintained. This does not mean that the chosen spokesperson has more power to make decision than other SDMs; it just simplifies the communication and provides both the family and the ICU team time and energy to focus on caring for the ill patient. As SDM or POA you may request a family meeting with the ICU team to further establish an understanding of the patients condition, and assist with your decision making.
Please ask your primary ICU nurse about setting up a Family/Patient meeting with the ICU team. Note that this may take time to arrange.
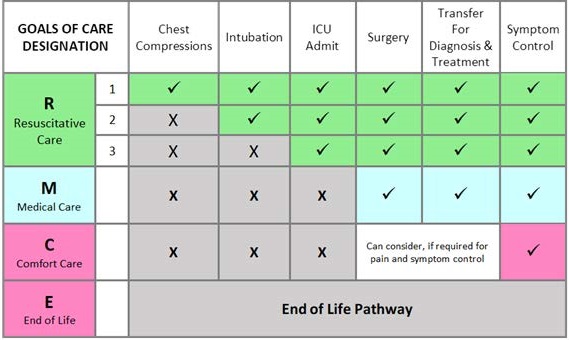
Goals of Care
The Goals of Care Designation order provides direction regarding specific health interventions, transfer decisions, locations of care and limitations on interventions for a patient as established after consultation between the most responsible physician and patient or substitute decision-maker where appropriate.
Goals of Care conversations ideally take place with the patient and whomever the patient chooses to be part of the conversation. If a patient has been found incapable of consenting to treatment, the patient’s substitute decision-maker must be approached in order to obtain consent to or refusal of treatment. These discussions should take place in person, whenever possible.
For more information about Goals of Care, please see our Patient Information Guidebook here.
Planning ahead
Before patient/substitute decision-maker meeting, health care team should review:
- Clarification of current medical status
- Clarification of team members expectations
- Degree of Benefit of treatment options
- Plan for the appropriate people to be present
- Choose the appropriate setting